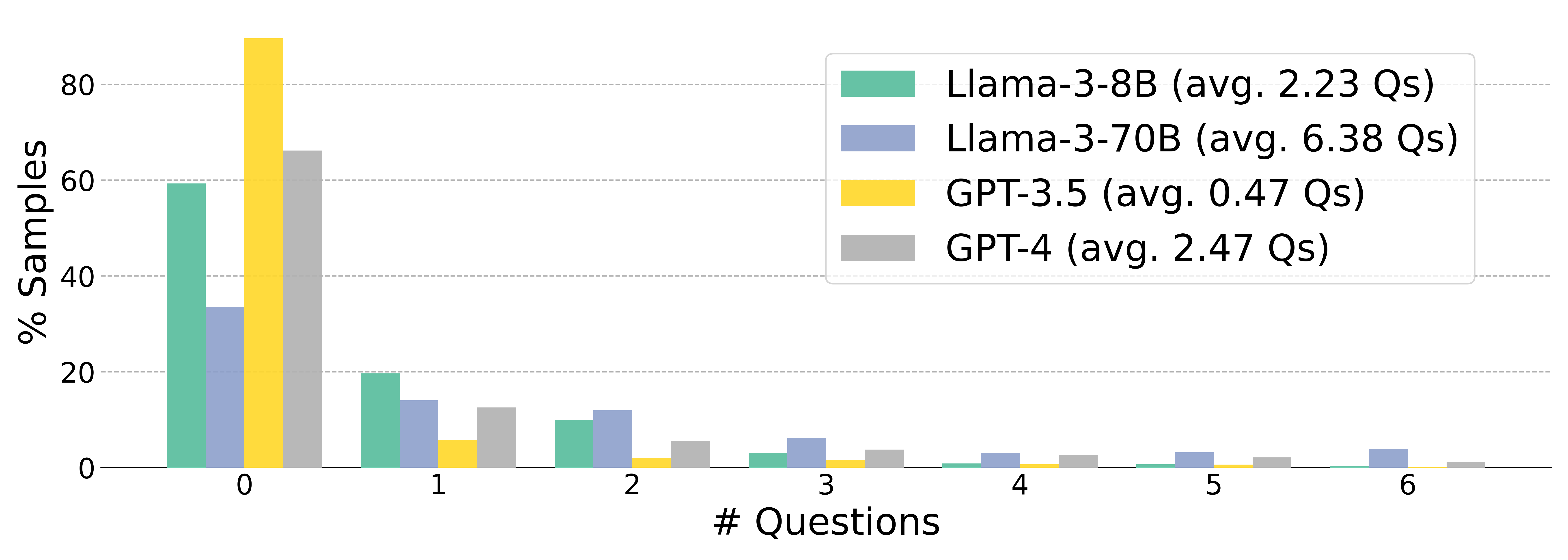
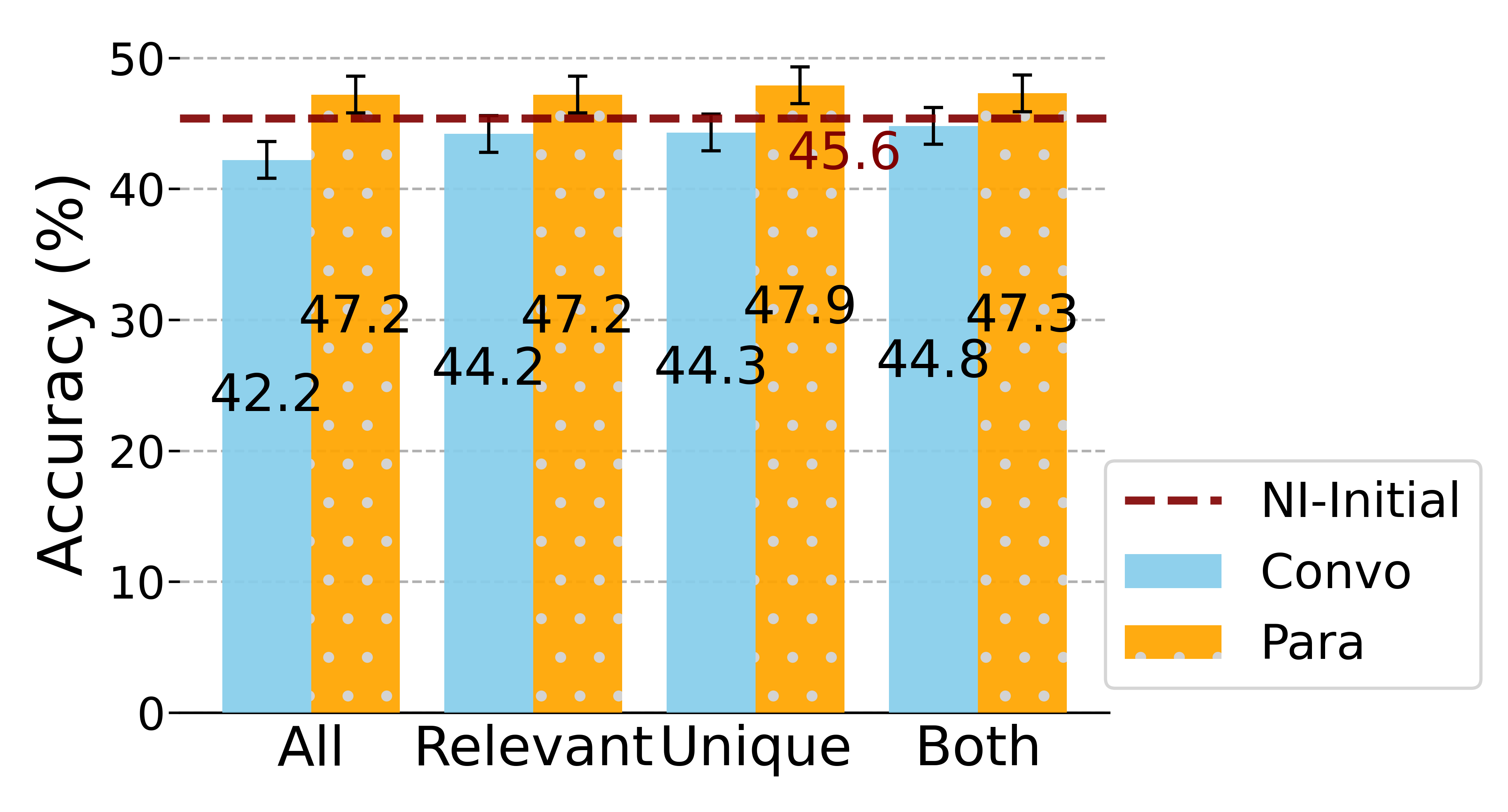
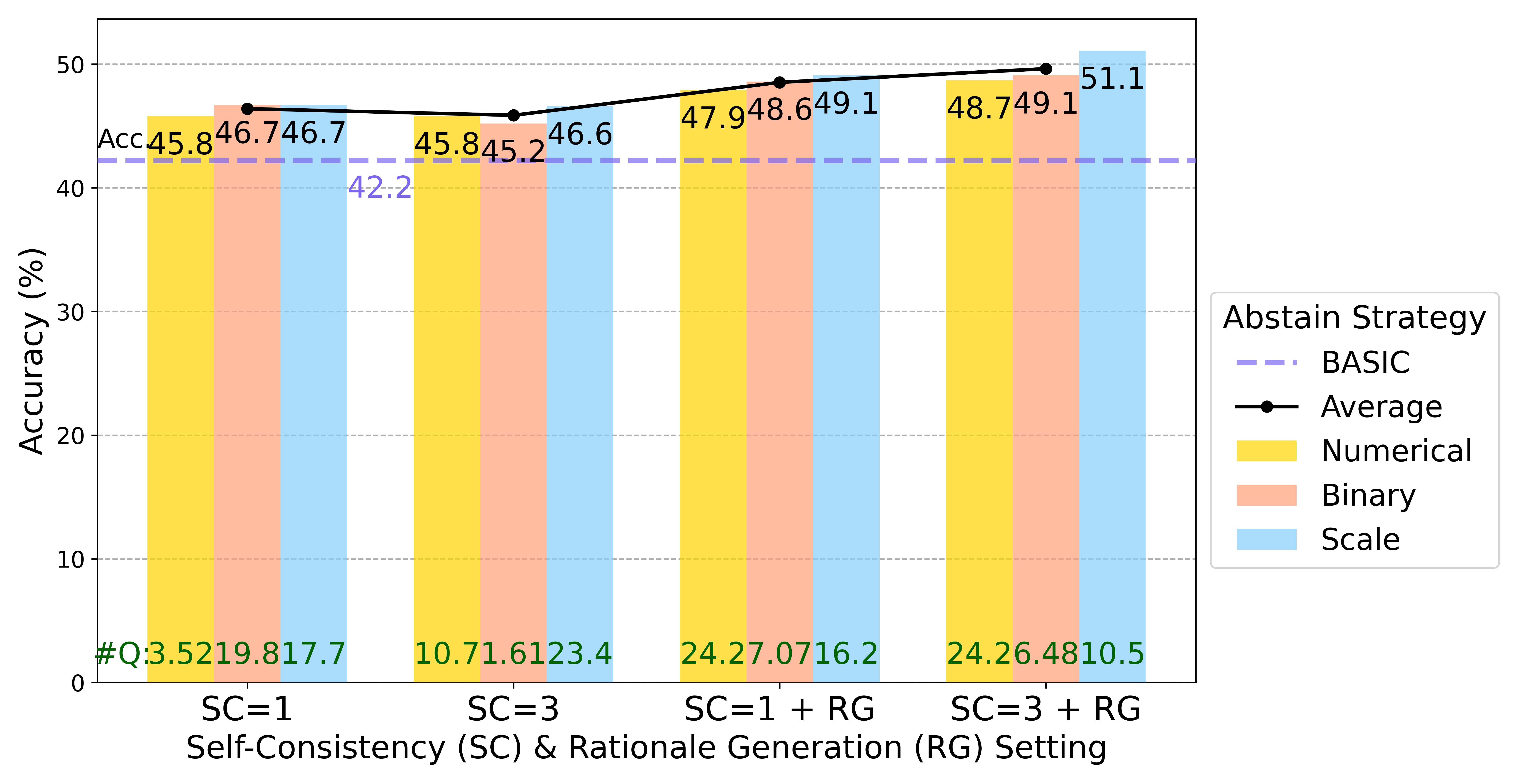
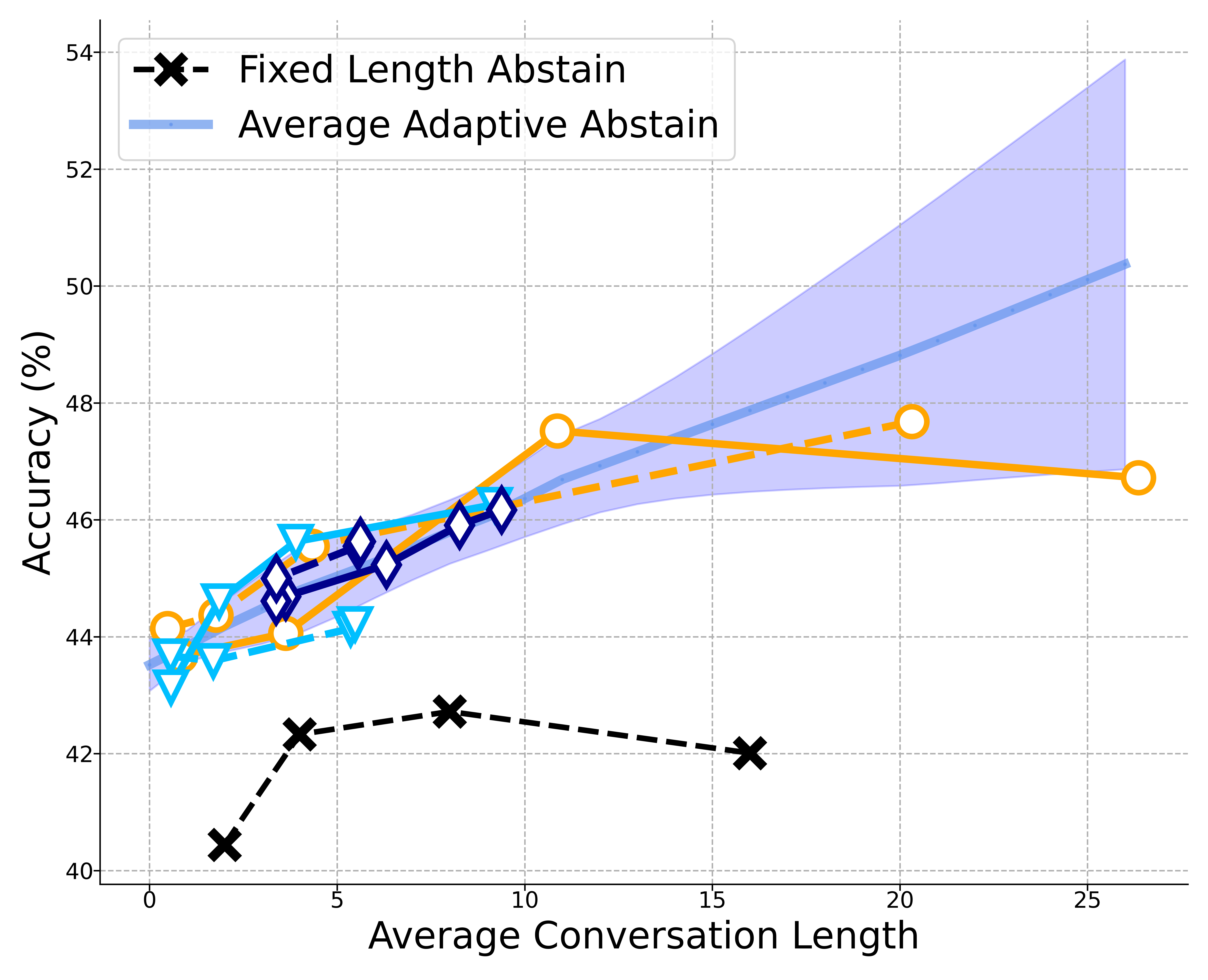
Users typically engage with LLMs interactively, yet most existing benchmarks evaluate them in a static, single-turn format, posing reliability concerns in interactive scenarios. We identify a key obstacle towards reliability: LLMs are trained to answer any question, even with incomplete context or insufficient knowledge. In this paper, we propose to change the static paradigm to an interactive one, develop systems that proactively ask questions to gather more information and respond reliably, and introduce an benchmark - MediQ - to evaluate question-asking ability in LLMs. MediQ simulates clinical interactions consisting of a Patient System and an adaptive Expert System; with potentially incomplete initial information, the Expert refrains from making diagnostic decisions when unconfident, and instead elicits missing details via follow-up questions. We provide a pipeline to convert single-turn medical benchmarks into an interactive format. Our results show that directly prompting state-of-the-art LLMs to ask questions degrades performance, indicating that adapting LLMs to proactive information-seeking settings is nontrivial. We experiment with abstention strategies to better estimate model confidence and decide when to ask questions, improving diagnostic accuracy by 22.3%; however, performance still lags compared to an (unrealistic in practice) upper bound with complete information upfront. Further analyses show improved interactive performance with filtering irrelevant contexts and reformatting conversations. Overall, we introduce a novel problem towards LLM reliability, an interactive MediQ benchmark and a novel question-asking system, and highlight directions to extend LLMs' information-seeking abilities in critical domains.
 MediQ: Question-Asking LLMs and a Benchmark for Reliable Interactive Clinical Reasoning
MediQ: Question-Asking LLMs and a Benchmark for Reliable Interactive Clinical Reasoning